RFK Jr. in the spotlight: vaccine panel upheaval, schedule review order, and a health agenda racing into year two
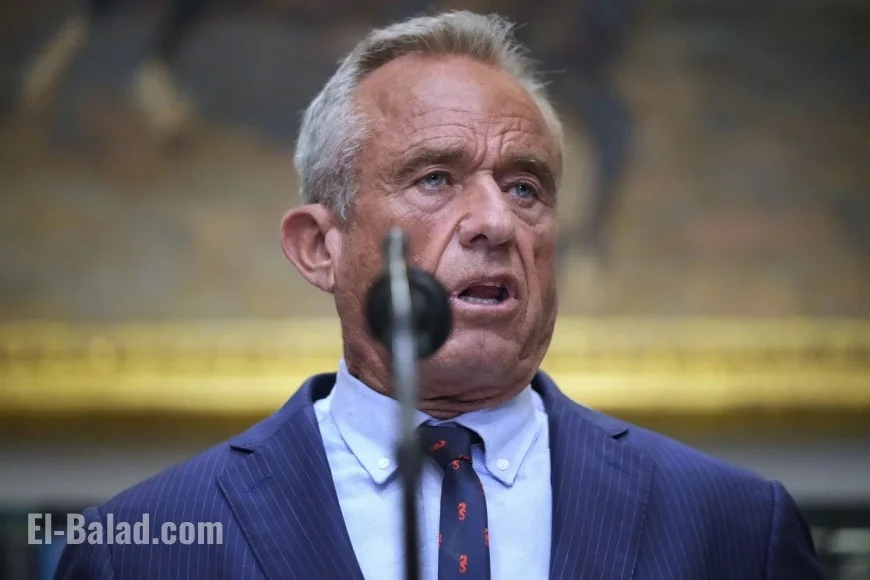
Robert F. Kennedy Jr., now serving as U.S. secretary of health and human services, is back at the center of the nation’s health debate after a cascade of developments in the past 24 hours. A federal advisory panel he empaneled advanced controversial changes to infant immunization policy, the White House pressed for an accelerated review of the childhood vaccine schedule, and public-health groups and patient advocates intensified pushback. The moves highlight how Kennedy’s “Make America Healthy Again” (MAHA) program is reshaping federal priorities—and how fiercely the scientific community plans to contest parts of it.
Vaccine headlines around RFK Jr.: what changed and what’s next
A key advisory committee aligned with HHS held a high-profile session on newborn immunizations and signaled support for revising the timing of the hepatitis B birth dose. The meeting, described by attendees as unusually contentious, ended with members preparing a formal recommendation path that could shift the first hepatitis B shot away from delivery for most newborns while keeping safeguards for infants at elevated risk. Final language has not been published, and agency officials cautioned that any change must clear additional scientific and legal steps before it can affect the national schedule. Recent updates indicate the matter remains fluid; parents and clinicians should expect further deliberation before policy hardens.
Compounding the stakes, the president directed HHS late last week to fast-track a review of the childhood vaccine schedule, with explicit comparisons to peer nations that administer fewer individual injections by grouping antigens differently. The order instructs Kennedy to deliver options on timing, combinations, and safety monitoring within an accelerated window, alongside an impact analysis on preventable-disease risk.
MAHA agenda: food, fitness, environment—and a widening AI footprint
While vaccines dominate headlines, Kennedy’s broader MAHA program continues to expand. The department recently outlined first-step plans to use artificial intelligence in screening paperwork bottlenecks, fraud detection, and clinical-trial matching—promising faster approvals for nutrition pilots and preventive-care grants. Separately, industry figures have publicly endorsed the MAHA emphasis on diet quality and ultra-processed foods, even as critics question conflicts in sectors that market high-sugar products. Expect more nutrition guidance trials, school-meal experiments, and primary-care pilots tied to lifestyle interventions in early 2026.
The criticism front: autism advocates, women’s health, and scientific norms
Kennedy’s long record of vaccine skepticism continues to animate opponents. Autism advocates intensified their campaigns in recent days, warning that changing long-standing immunization norms—without overwhelming new evidence—could depress uptake and risk outbreaks. Women’s-health groups, meanwhile, are pressing HHS for clear commitments on menopause care, maternal health, and access to evidence-based treatments, arguing that preventive services deserve as much urgency as schedule rewrites and nutrition policy.
Public-health leaders also raised alarms about process: who selects advisory members, how conflicts are disclosed, and whether meetings allow adequate time for external data and stakeholder testimony. HHS officials have defended the committees as lawful and diverse in perspective, while acknowledging that unusually high public interest has strained normal procedures.
What matters for parents, clinicians, and schools right now
-
No immediate change at the bedside: Until HHS publishes finalized recommendations and the immunization schedule is formally updated, hospitals and pediatric practices keep current protocols.
-
Documentation will be key: If revisions proceed, expect detailed risk-stratification for the hepatitis B birth dose and clear catch-up pathways; birthing centers and NICUs will need updated consent and screening workflows.
-
Communication burden rises: Pediatricians and school nurses should prepare plain-language materials to address hesitancy, especially in districts where vaccine requirements intersect with enrollment deadlines.
-
Supply and coding checks: Any re-timing or combination-shot pivot ripples through inventory, billing codes, and payer policies. Practices should monitor payer bulletins closely.
Political calculus: why RFK Jr. dominates the health narrative
As a cabinet official with celebrity-level name recognition, Kennedy can marry agency levers (advisory panels, grantmaking, guidance) with a media megaphone. The dynamic ensures outsized attention to vaccination debates even as HHS pursues quieter MAHA planks on food policy, environmental exposures, and primary-care access. For the administration, accelerating the schedule review satisfies a campaign promise to “re-examine the science,” while handing opponents a rallying point to defend longstanding evidence.
What to watch in the coming days
-
Draft text from the vaccine advisory panel: The specificity of risk categories and hospital workflows will reveal how sweeping the proposed hepatitis B changes really are.
-
HHS timetable for the schedule review: Look for milestones—public comment periods, data-sharing sessions, and safety-surveillance reports.
-
Provider groups’ formal statements: Endorsements or rebukes from pediatric and infectious-disease societies will shape state-level policy and school requirements.
-
MAHA funding announcements: New pilots on nutrition, fitness, and environmental health could arrive before year-end, offering a counterweight to the vaccine fight.
-
Litigation watch: If opponents argue process violations, court challenges could slow or freeze any adopted changes.
Bottom line: RFK Jr.’s HHS is moving quickly on its signature themes—diet and chronic disease prevention—while reopening the nation’s most emotionally charged public-health debate. With a newborn-vaccine recommendation in flux and a compressed review of the childhood schedule now ordered, the outcome will hinge on how convincingly HHS can show that any revisions preserve the core promise of modern immunization: fewer preventable diseases, not more.