State Mental Hospitals Face Systemic Failures, Resembling Prisons
State mental hospitals across the United States are experiencing significant challenges, resembling prisons rather than centers for healing. This trend has been particularly evident in Ohio, where families like that of Quincy Jackson III struggle to navigate a system marked by neglect and inadequate resources.
Systemic Failures in Mental Health Care
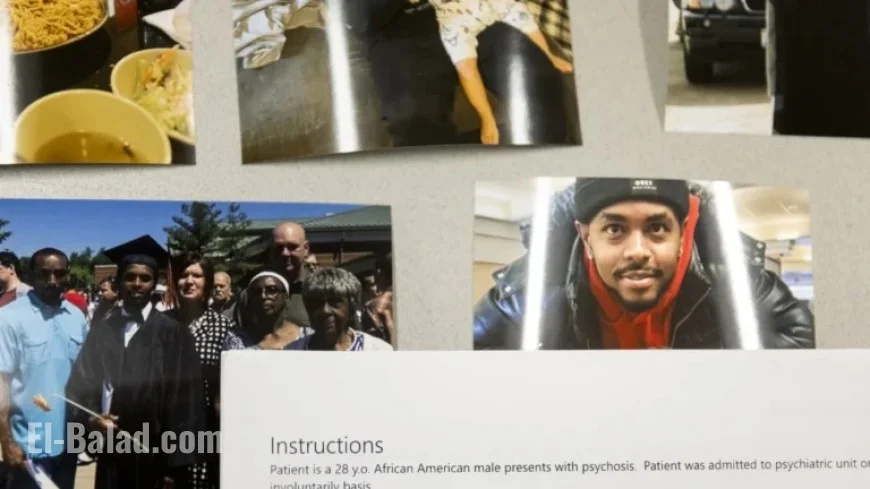
Many families feel the mental health system criminalizes individuals with serious mental illnesses rather than supporting them. Tyeesha Ferguson fears for her 28-year-old son, Quincy, who has been entangled in cycle of hospitalizations and jails for nearly a decade.
Over recent years, the share of patients with criminal charges in Ohio’s state hospitals has sharply risen. In 2002, about half of state hospital patients had criminal charges; today, this figure is around 90%. Simultaneously, the total number of patients in these hospitals has declined by 50%, from 6,809 in 2002 to just 3,421 in recent figures from the U.S. Substance Abuse and Mental Health Services Administration.
Patient Wait Times and Overcrowding
Across the nation, psychiatric hospitals are grappling with severe understaffing and increasing numbers of patients awaiting care. Many facilities are forced to turn away individuals or leave them waiting for extended periods. In Ohio, the median wait time for a state hospital bed reached 37 days in May 2024, a significant delay for those requiring urgent treatment.
- In 2018, state officials noted severe bed shortages in Ohio.
- Recent assessments indicated that the six regional psychiatric hospitals in Ohio provide about 1,100 beds.
- A significant increase in patients with criminal charges has further strained hospital resources.
Effect of Legislation on Mental Health Services
Legislation affecting federal Medicaid budgets has further squeezed local mental health services, many of which serve uninsured patients or those on Medicaid. The passing of the One Big Beautiful Bill Act has been particularly damaging, proposing a nearly $1 trillion cut to Medicaid over the next ten years.
Retired Ohio Supreme Court Justice Evelyn Lundberg Stratton highlighted the urgent crisis in mental health care, noting that families are suffering as they seek hospital beds for loved ones outside the criminal justice system. “It hurts everybody who has someone who needs to get a hospital bed,” Stratton stated.
Life Inside Today’s Psychiatric Facilities
The shift towards accommodating more criminally charged patients has drastically affected the environment in psychiatric hospitals. Increased restrictions and reduced care quality have become common, creating a sense of tension among patients and staff alike.
High-profile incidents of violence connected to inadequate mental health care have caught national attention, raising questions about systemic failures. Reported events include stabbings and assaults committed by individuals with known mental health issues, illustrating the dire need for better treatment options.
Inadequate Staffing and Safety Concerns
As psychiatric facilities become more restrictive due to the influx of patients with criminal charges, safety concerns for both patients and staff have worsened. Reports from 2019 and 2020 indicated alarming circumstances, including patient suicides and deaths linked to understaffing.
- A federal lawsuit has been filed alleging abuse and neglect in state hospitals.
- Feedback from former staff emphasizes the dangerous conditions resulting from a lack of personnel and resources.
Long Waits for Treatment
Being unable to receive timely mental health treatment exacerbates symptoms for individuals like Quincy Jackson III, who described how time spent in jail without medication worsened his condition. The consequences of delayed treatment can lead to cycles of incarceration or violence that could otherwise be avoided with appropriate care.
A Path Forward
To address the systemic failures in mental health care, experts and advocates are calling for comprehensive reforms. They emphasize the importance of increasing resources for mental health services and transforming state psychiatric hospitals into safe places for healing rather than incarceration.
Ohio officials are initiating plans to expand treatment options and invest in new psychiatric facilities. However, advocates warn that simply increasing bed capacity is insufficient without systemic changes to improve care quality and access.
Families like Tyeesha Ferguson’s seek assurance that their loved ones will receive the treatment they need without being swept into the criminal justice system. “He’s not a throwaway child,” she asserts, echoing the sentiments of many who confront the challenges of systemic failures in mental health care.